Infection Control – It’s in Your Hands!
Infection control is important because it is the best way that we can prevent the spread of many common contagious diseases. The following piece discusses effective methods of infection control, particularly with regard to schools and daycare centers.
What are infections?
How do we get infections?
What is the best way to wash your hands for proper infection control?
How long do you need to wash your hands for good infection control?
When should you wash your hands to prevent infection?
What are the best ways to control the spread of infections in schools?
When do children need to be excluded from day care or school in order to help with infection control?
What are infections?
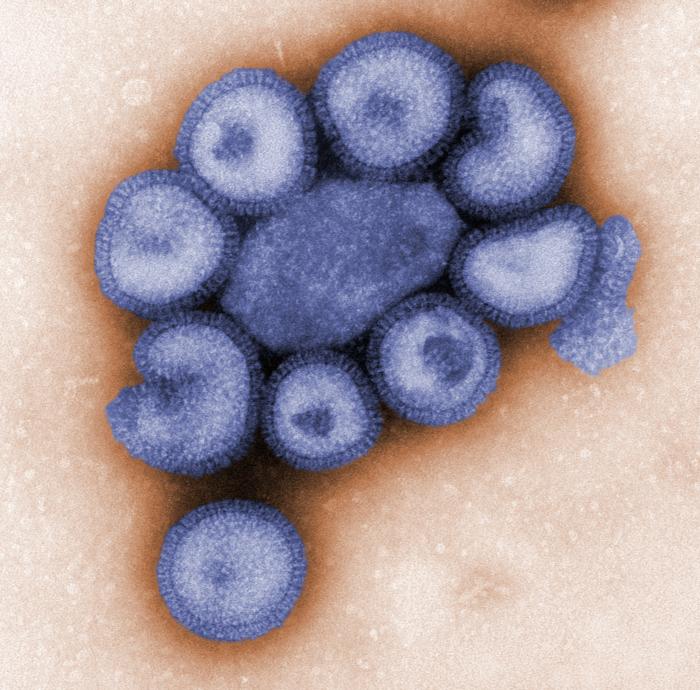
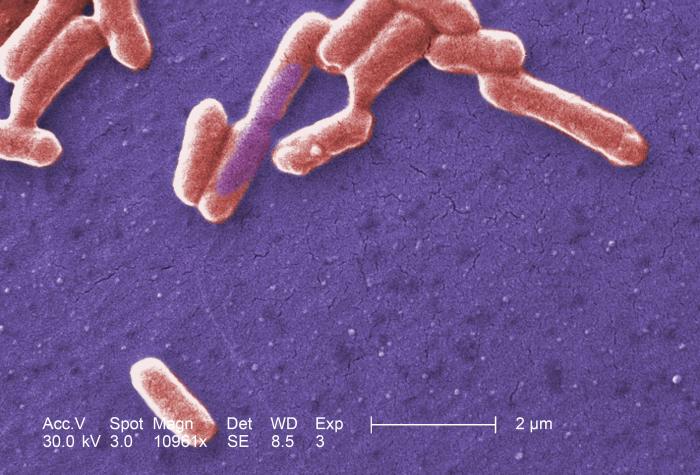
Infections are caused by germs within our bodies that shouldn’t be there. Viruses, bacteria, fungi, and parasites are all different categories of germs which each cause different types of infections.
 |
 |
 |
 |
| Viruses – These influenza virus particles or “virions” cause the contagious respiratory illness known as flu. | Bacteria – E. coli 0157:H7 can cause foodborne illness, bloody diarrhea, kidney failure, and sometimes death. |
Fungi – This fungus, Penicillium marneffei, usually affects those with AIDS or undergoing chemotherapy. |
Parasites – Giardia lamblia infection can occur from contaminated water, food, or by the fecal-oral route. |
How do we get infections?
Viruses, bacteria, fungi, or parasites can be spread when a sick person coughs into the air or by touching that person’s secretions (urine, runny nose, cough, and diarrhea). Drinking or eating after an ill person or handling items that they have touched are common ways you can come into contact with these secretions. When the germ particles enter your body, they can cause you to have an infection.
Since MOST infections are spread by touch, washing your hands before touching another person is one of the best ways to help stop the spread of infections. However, it is important to wash your hands even when you are not feeling sick because most germs are actually transmitted a few days BEFORE you start feeling sick.
What is the best way to wash your hands for proper infection control?
The Henry the Hand Campaign seeks to educate the public on 4 important principles of good 
1) WASH your hands when they are dirty and BEFORE eating.
2) DO NOT cough into your hands.
3) DO NOT sneeze into your hands.
4) DO NOT put your fingers into your eyes, nose or mouth.
(Source:http:// http://www.henrythehand.com/)
** Regular soap and water are best. Antibacterial soaps are not necessary if you have spent enough time (at least 20 seconds) cleaning your hands with regular soap and water.
How long do you need to wash your hands for good infection control?
The answer is 20 seconds. Singing a song like “Happy Birthday” twice while cleaning your hands with soap and water helps to assure that you have spent the correct amount of time required to actually kill the germs on your hands.
When should you wash your hands to prevent infection?
1. Before preparing or eating food
2. After going to the bathroom
3. After changing diapers
4. Before and after tending to someone who is sick
5. After blowing your nose, coughing, or sneezing
6. After handling animal waste
7. After handling garbage
8. Before and after treating a cut or wound
(Source: http://www.cdc.gov/cleanhands/)
What are the best ways to control the spread of infections in schools?
School attendance is important. However, sick children in crowded schools can also lead to the spread of infections to healthy children. The following guidelines are noted by the American Academy of Pediatrics for schools regarding infection control:
1. Immunizations. Although specific laws vary by state, most states require proof of protection against:
- Diphtheria
- Measles
- Mumps
- Pertussis
- Poliomyelitis
- Rubella
- Tetanus
- Hepatitis A virus immunization is recommended.
- Hepatitis B virus immunization is recommended.
- Meningococcal immunization is recommended.
- Varicella (chicken pox) immunization is recommended.
For a list of mandatory immunizations by state that are required to attend school and/or daycares see the following websites: www.immunize.org/laws or www.cdc.gov/other.htm#states. Policies established by each state’s health department about exclusions of un-immunized children and exemptions for children with certain underlying medical conditions and families with religious or philosophic objection to immunization should be followed.
2. Infected children should be excluded from school until they no longer are considered contagious. (For recommendations, see When do children need to be excluded from day care or school in order to help with infection control? in next section.)
3. In some instances, administration of appropriate antibiotics to the sick child will limit further spread of infection (for example, antibiotics for streptococcal throat infection and antibiotics for pertussis or ‘whooping cough’).
4. Appropriate antibiotic prevention should be given to close contacts of children with infections caused by specific pathogens (for example, close contacts of a child diagnosed with meningococcal bacterial meningitis).
5. Temporary school closing can be used in limited circumstances:
- When an infection is expected to affect a large number of susceptible students and available control measures are considered inadequate (for example, a large outbreak of influenza)
- When an infection is expected to have a high rate of morbidity or mortality (for example, several cases of meningococcal bacterial meningitis)
**In all circumstances requiring intervention to prevent spread of infection within the school setting, the privacy of children who are infected should be protected.
(Source for above school recommendations: School Health Section, American Academy of Pediatrics Red Book 2006: pages 145-146)
When do children need to be excluded from day care or school in order to help with infection control?
Mild illness is common among children. Most children will not need to be excluded from school or their usual 
However, during the course of an identified outbreak of any communicable illness in a childcare setting or school, a child determined to be contributing to transmission of organisms causing the illness may be excluded. In general, the child may be readmitted when the risk of transmission is determined no longer to be present.
Children should be kept out of the childcare setting or school for the following:
- Illness that prevents the child from participating comfortably in common program activities
- Illness that results in a need for care that is greater than the staff can provide without compromising the health and safety of the other children
- Any of the following conditions suggesting possible severe illness:
- fever accompanied by behavior changes
- lethargy
- irritability
- persistent crying
- difficult breathing
- other manifestations of possible severe illness, such as a quickly spreading rash
- Diarrhea that contains blood or mucus
- Mouth sores associated with drooling, unless the child’s physician or local health department authority states that the child is non-infectious
- Persistent abdominal pain (continues for longer than 2 hours) or intermittent abdominal pain associated with fever or dehydration
- Rash with fever or behavioral change, until a physician has determined the illness is not a communicable disease
- Vomiting 2 or more times during the previous 24 hours, unless the vomiting is determined to be caused by a non-communicable condition and the child is not in danger of dehydration
- Purulent conjunctivitis (defined as pink or red conjunctiva with white or yellow eye discharge, often with matted eyelids after sleep and eye pain or redness of the eyelids or skin surrounding the eye), until examined by a physician and approved for readmission
- Shiga toxin-producing Escherichia coli, including E. coli O157:H7, or Shigella infection, until diarrhea resolves and results of 2 stool cultures are negative for these organisms
- Head lice (pediculosis), at the end of the program or school day and until after the first treatment
- Hepatitis A virus infection, until 1 week after onset of illness or jaundice (if symptoms are mild)
- Impetigo, until 24 hours after treatment has been initiated
- Measles, until 4 days after onset of rash
- Mumps, until 9 days after onset of parotid gland swelling
- Pertussis, until 5 days of appropriate antimicrobial therapy have been completed
- Rubella, until 6 days after onset of rash
- Salmonella infection, until diarrhea resolves and 3 stool cultures test negative for Salmonella typhi; other types of Salmonella infection do not require negative stool culture results
- Scabies, until after treatment has been given
- Strep throat (Streptococcal pharyngitis), until 24 hours after treatment has been initiated
- Tuberculosis, until the child’s physician or local health department authority states that the child is non-infectious
- Varicella (chicken pox), until all lesions have dried and crusted (usually 6 days after initial onset of rash)
Most minor illnesses do not constitute a reason for excluding a child from childcare. Examples of illnesses and conditions that do not necessitate exclusion include the following:
- Non-purulent conjunctivitis (defined as pink conjunctiva with a clear, watery eye discharge without fever, eye pain, or eyelid redness)
- Cytomegalovirus (CMV) infection
- Chronic hepatitis B virus (HBV) infection
- Human immunodeficiency virus (HIV) infection
- Parvovirus B19 infection (Fifth disease) in an immunocompetent and otherwise healthy host
- Rash without fever and without behavioral change
Asymptomatic children with mild loose stools usually do not need to be excluded, except when an infection with Shiga toxin-producing E. coli or with Shigella species has occurred in the child care program or school. Because these infections are transmitted easily and can be severe, exclusion is warranted until results of 2 stool cultures are negative for the organism.
Source: Recommendations for Inclusion or Exclusion, American Academy of Pediatrics Red Book 2006: pages 133-135.
For Parents:
School and Illness: Should Your Child Stay Home? (pdf)
For more information:
Go to the Infectious Diseases health topic.