Healthy Kids Healthy Weight: Where We Are & What We Can Do
Healthy Kids Healthy Weight: Where We Are & What We Can Do

- More than one out of three adults in the United States are obese.
- Medical costs related to obesity were about $147 billion in 2008 and continue to rise.
Children and teens are also becoming overweight and obese at an alarming rate. In 2010, the CDC found that more than a third of children were overweight or obese. See Childhood Obesity Facts. This raises new concern. Diseases that were previously ‘adult diseases’ are now affecting children and teens. For example, type 2 diabetes has increased parallel to the rise in childhood obesity. The hidden damage to the body starts much earlier in life. This can result in serious harm like heart disease and vision loss at a younger age.
How are Overweight and Obesity Defined?
Definitions of overweight and obesity are important to understand. They can also be confusing in children.
-
Overweight is defined as having too much weight for a particular height. That extra weight can be from
- fat
- muscle
- bone
- water
- or a combination of these factors.
- Obesity is defined as having too much body fat.
Body Mass Index, also called BMI, uses a person’s weight and height to calculate a new number. That BMI number is a way to tell how much body fat a person has. It shows whether a person is overweight and at risk for future health problems.
Overweight and Obesity in Children and Teens
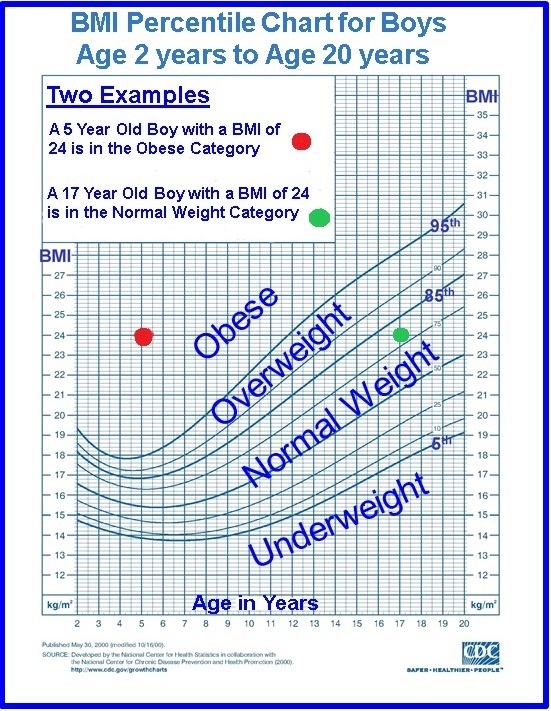
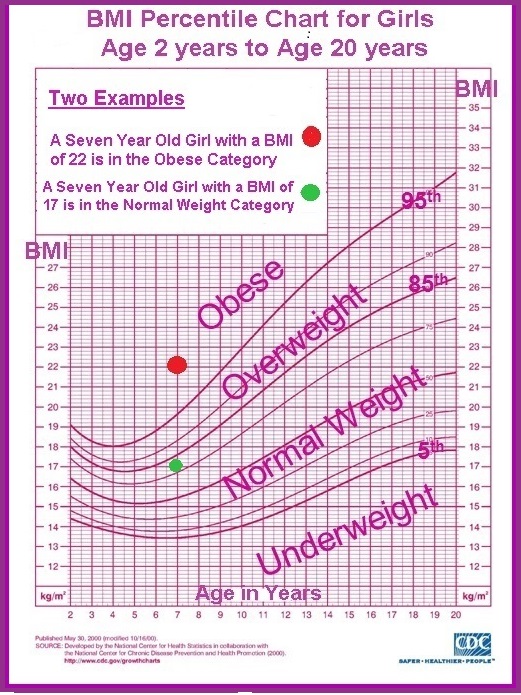
Children and teens need a special tool to show if their BMI is in an overweight or obese group. This tool is a “BMI-for-age percentile.” It is used because:
- The amount of body fat that is normal changes with age.
- The amount of body fat is different for girls and boys.
The same BMI number may be obese for a younger child and normal for an older child. Or, a boy might be obese and a girl not obese even though their BMIs are exactly the same BMI scores used for adults have little meaning for children and teens. You can get information on BMI and what it means the CDC’s page about BMI for Children and Teens.
BMI Percentile Charts and Examples
Special BMI percentile charts take this all into account. There is one chart for girls and another chart for boys. Knowing your child’s BMI is the starting point.
When the BMI number is entered for the age of the child, the chart shows if they are underweight, normal weight, overweight or obese.
Normal Weight: BMI between 5th and 85th percentile
This means that a child has a normal weight if their BMI is between 5 percent and 85 percent of all children who are the same sex and age.
Overweight: BMI between 85th and 95th percentile
This means that a child is overweight if their BMI is between 85 percent and 95 percent of all children who are the same sex and age.
Obese: BMI equal to or above the 95th percentile
This means that a child is obese if their BMI is the same or higher than 95 percent of all children who are the same sex and age.
You can see 2 BMI Percentile Charts with examples below. There is one for girls and one for boys. The first chart shows BMI numbers for 2 seven year old girls who have different BMI numbers. The girl with a BMI number of 17 falls in the normal weight group and the girl with a BMI number of 22 is in the obese group. The second chart shows a 5 year old boy and a 17 year old boy with the same BMI number: 24. That puts the 17 year old boy in the normal weight group and the 5 year old boy in the obese group.
 |
 |
|
These charts have been modified from the National Center for Health Statistics charts “2 to 20 years: Boys Body mass index-for-age percentiles” and “2 to 20 years: Girls Body mass index-for-age percentiles”. |
|
Do-it-Yourself BMI Calculator
The CDC has a special Do-it-Yourself BMI Calculator that does it all for you. Once you enter information the calculator:
- Calculates the BMI number
- Tells you if that BMI is at a healthy weight, overweight or obese
- Explains what that means
- Describes what to do
What Causes Overweight and Obesity?
Eating more calories than you use in activity causes overweight and obesity. Many people believe that obesity is inherited. That is actually very rare. A few medical conditions can cause weight gain in children. These include low thyroid hormone, called “hypothyroidism,” and too much cortisol, called “Cushing syndrome.” Medical causes are not common and are detected by laboratory tests.
Most of the time, overweight and obesity are caused by:
- Extra calories from food, snacks or sugary drinks
- Not enough activity or exercise
The diet and activity of children and teens is strongly influenced by:
- Where they live and go to school
- Family budget and shopping choices
- Food preparation: tradition and culture
- Food Marketing: media and advertisements
Are There Emotional Effects?
When children and teens are overweight or obese, it affects confidence and self esteem. It is important for parents, teachers and providers to be aware of these needs. It is also important not to ignore childhood obesity.
What Can Families & Communities Do?
There are efforts to limit marketing of unhealthy foods to children. Many schools ban soda machines. Some schools have healthier menu options for school lunches. More school programs increase exercise and activity. Cities have increased availability of fresh fruits and vegetables. Communities have made safe places for exercise. Much work remains to be done, especially in our inner cities.
Education about healthy weight is extremely important. Current efforts include communities, schools churches and social media. Healthy eating and activity are promoted. Education outreach to school nurses and doctors supports tracking BMI. This improves detection and care of children at risk
|
Points to Remember:
|
Hope through Research
Many research studies are underway to help us learn about overweight and obesity in children. Would you like to learn more about being part of this exciting research? Please visit the following links:
- No More Hand-Me-Down Research (NIH)
- Research Studies for Children and Teenagers
- Should Your Child Be in a Clinical Trial? (FDA.gov)
- Your Child Can Help Find Cures at the NIH Clinical Center (NIH)
- Children’s Assent to Clinical Trial Participation (NIH)
This children’s health content is brought to you with support from University Hospitals Rainbow Babies & Children’s Hospital.
For more information:
Go to the Kids’ Healthy Weight health topic.